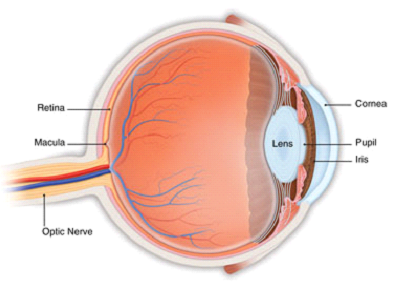
Age-related macular degeneration (AMD) is a deterioration or breakdown of the eye's macula. The macula is a small area in the retina - the light-sensitive tissue lining the back of the eye. The macula is the part of the retina that is responsible for your central vision, allowing you to see fine details clearly.
The macula makes up only a small part of the retina, yet it is much more sensitive to detail than the rest of the retina (called the peripheral retina). The macula is what allows you to thread a needle, read small print, and read street signs. The peripheral retina gives you side (or peripheral) vision. If someone is standing off to one side of your vision, your peripheral retina helps you know that person is there by allowing you to see their general shape.
Many older people develop macular degeneration as part of the body's natural aging process. There are different kinds of macular problems, but the most common is age-related macular degeneration.
With macular degeneration, you may have symptoms such as blurriness, dark areas or distortion in your central vision, and perhaps permanent loss of your central vision. It usually does not affect your side, or peripheral vision. For example, with advanced macular degeneration, you could see the outline of a clock, yet may not be able to see the hands of the clock to tell what time it is.
Causes of macular degeneration include the formation of deposits called drusen under the retina, and in some cases, the growth of abnormal blood vessels under the retina. With or withouttreatment, macular degeneration alone almost never causes total blindness. People with more advanced cases of macular degeneration continue to have useful vision using their side, or peripheral vision. In many cases, macular degeneration's impact on your vision can be minimal.
When macular degeneration does lead to loss of vision, it usually begins in just one eye, though it may affect the other eye later.
Many people are not aware that they have macular degeneration until they have a noticeable vision problem or until it is detected during an eye examination.
There are two types of macular degeneration:
Most people who have macular degeneration have the dry form. This condition is caused by aging and thinning of the tissues of the macula. Macular degeneration usually begins when tiny yellow or white pieces of fatty protein called drusen form under the retina. Eventually, the macula may become thinner and stop working properly.
With dry macular degeneration, vision loss is usually gradual. People who develop dry macular degeneration must carefully and constantly monitor their central vision. If you notice any changes in your vision, you should tell your ophthalmologist right away, as the dry form can change into the more damaging form of macular degeneration called wet (exudative) macular degeneration. While there is no medication or treatment for dry macular degeneration, some people may benefit from a vitamin therapy regimen for dry macular degeneration.
Using an Amsler grid to test for macular degeneration
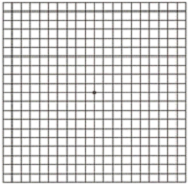
If you have been diagnosed with dry macular degeneration, you should use a chart called an Amsler grid every day to monitor your vision, as dry macular degeneration can change into the more damaging wet form.
To use the Amsler grid, wear your reading glasses and hold the grid 12 to 15 inches away from your face in good light.
About 10 percent of people who have macular degeneration have the wet form, but it can cause more damage to your central or detail vision than the dry form.
Wet macular degeneration occurs when abnormal blood vessels begin to grow underneath the retina. This blood vessel growth is called choroidal neovascularization (CNV) because these vessels grow from the layer under the retina called the choroid. These new blood vessels may leak fluid or blood, blurring or distorting central vision. Vision loss from this form of macular degeneration may be faster and more noticeable than that from dry macular degeneration.
The longer these abnormal vessels leak or grow, the more risk you have of losing more of your detailed vision. Also, if abnormal blood vessel growth happens in one eye, there is a risk that it will occur in the other eye. The earlier that wet macular degeneration is diagnosed and treated, the better chance you have of preserving some or much of your central vision. That is why it is so important that you and your ophthalmologist monitor your vision in each eye carefully.
In its earliest stages, people may not be aware they have macular degeneration until they notice slight changes in their vision or until it is detected during an eye exam. People who are at risk for macular degeneration should have regular eye exams to test for macular degeneration and, if diagnosed, begin treatment if appropriate.
Dry macular degeneration can affect one or both eyes. You may not notice vision changes if only one eye is affected, as your unaffected eye will compensate for vision loss in the other eye.
Wet macular degeneration symptoms usually appear and get worse fairly quickly.
Recently much new information on macular degeneration has been discovered. Genetic changes appear to be responsible for approximately half the reason for individuals getting macular degeneration. Additionally, there are other risk factors for developing the disease. Many older people develop macular degeneration as part of the body's natural aging process. One large study found that the risk of getting macular degeneration jumps from about 2 percent of middle-aged people in their 50s to nearly 30 percent in people over age 75.
Our bodies constantly react with the oxygen in our environment. Over our lifetimes, as a result of this activity, our bodies produce tiny molecules called free radicals. These free radicals affect our cells, sometimes damaging them. This is called oxidative stress and is thought to play a major role in how macular degeneration develops. Approximately 1 in 3 Caucasians have genetic changes that make them more prone to damage from oxidative stress, which can lead to macular degeneration.
Heredity is another risk factor for macular degeneration. People who have a close family member with the disease have a greater chance of developing macular degeneration themselves.
Some studies have shown that inflammation (swelling of the body’s tissues) may play a role in macular degeneration development. Inflammation is the way the body’s immune system fights off infection or other things it considers “invaders.” But an overactive immune system with its associated inflammation may be a risk factor for macular degeneration.
Smoking and high blood pressure are associated with the wet form of macular degeneration. Research also suggests there may be a link between being obese and having early or intermediate-stage macular degeneration develop into the advanced (wet) form.
Another risk factor for developing macular degeneration may include having abnormal cholesterol levels or having high blood pressure (called hypertension).
Many people do not realize they have a macular problem until they notice they have blurred or distorted vision. Regular eye exams by an ophthalmologist may help to detect problems or early stages of macular degeneration before you are even aware of them.
To check for macular degeneration, your eye doctor will dilate (widen) your pupils using eyedrops and examine your eyes with an ophthalmoscope, a device that allows him or her to see the retina and other areas at the back of the eye. If macular degeneration is detected, your doctor may have you use an Amsler grid to check for macular degeneration symptoms such as wavy, blurry or dark areas in your vision.
If your ophthalmologist suspects you may have the wet form of macular degeneration, he or she will take special photographs of your eye with fluorescein angiography and optical coherence tomography (OCT). OCT scanning is a sophisticated and exact tool that detects abnormal blood vessels by creating a special picture of your macula.
During fluorescein angiography, a fluorescein dye is injected into a vein in your arm. The dye travels throughout the body, including your eyes. Photographs are taken of your eye as the dye passes through the retinal blood vessels. Abnormal areas will be highlighted by the dye, showing your doctor whether wet macular degeneration treatment is possible and, if so, where to treat the abnormal vessels.
Unfortunately, at this time there is no single proven treatment for the dry form of macular degeneration. However, a large scientific study has shown that antioxidant vitamins and zinc may reduce the impact of macular degeneration in some people by slowing its progression toward more advanced stages.
The Age-Related Eye Disease Study 2 (AREDS2) showed that among people at high risk for developing late-stage, or wet, macular degeneration (such as those who have large amounts of drusen or who have significant vision loss in at least one eye), taking a dietary supplement of vitamin C, vitamin E, lutein and zeaxanthin, along with zinc, lowered the risk of macular degeneration progressing to advanced stages by at least 25 percent. The supplements did not appear to provide a benefit for people with minimal macular degeneration or people without evidence of the disease during the course of the study.
Following is the nutrient supplementation shown to be beneficial in lowering the risk of macular degeneration progressing to advanced stages:
Another large study in women showed a benefit from taking folic acid and vitamins B6 and B12. Other studies have shown that eating dark leafy greens, and yellow, orange and other colorful fruits and vegetables, rich in lutein and zeaxanthin, may reduce your risk for developing macular degeneration.
These vitamins and minerals are recommended in specific daily amounts in addition to a healthy, balanced diet. Some people may not wish to take large doses of antioxidants or zinc because of medical reasons.
It is very important to remember that vitamin supplements are not a cure for macular degeneration, nor will they give you back vision that you may have already lost from the disease. However, specific amounts of these supplements do play a key role in helping some people at high risk for developing advanced (wet) AMD to maintain their vision, or slow down the progression of the disease.
Talk with your ophthalmologist to find out if you are at risk for developing advanced macular degeneration, and to learn if supplements are recommended for you.
Treating the wet form of macular degeneration may involve the use of anti-VEGF treatment, thermal laser treatment or photodynamic therapy (PDT). Treatment of wet macular degeneration generally reduces—but does not eliminate-- the risk of severe vision loss.
A common way to treat wet macular degeneration targets a specific chemical in your body that causes abnormal blood vessels to grow under the retina. That chemical is called vascular endothelial growth factor, or VEGF. Several new drug treatments (called anti-VEGF drugs) have been developed for wet AMD that can block the trouble-causing VEGF. Blocking VEGF reduces the growth of abnormal blood vessels, slows their leakage, helps to slow vision loss, and in some cases improves vision.
Your ophthalmologist administers the anti-VEGF drug (such as Avastin, Lucentis, and Eylea) directly to your eye in an outpatient procedure. Before the procedure, your ophthalmologist will clean your eye to prevent infection and will use an anesthetic drop or injection of anesthetic with a very fine needle to numb your eye. You may receive multiple anti-VEGF injections over the course of many months. Repeat anti-VEGF treatments are often needed for continued benefit.
In some cases, your ophthalmologist may recommend combining anti-VEGF treatment with other therapies. The treatment that’s right for you will depend on the specific condition of your macular degeneration.
Although most cases of wet AMD are treated with medication, in some instances thermal laser therapy may be used. Laser treatment is usually done as an outpatient procedure in the doctor’s office or at the hospital.
The laser beam in this procedure is a high-energy, focused beam of light that produces a small burn when it hits the area of the retina to be treated. This destroys the abnormal blood vessels, preventing further leakage, bleeding and growth.
Following laser treatment, vision may be more blurred than before treatment, but often it will stabilize within a few weeks. A scar forms where the treatment occurred, creating a permanent blind spot that might be noticeable in your field of vision.
Usually the abnormal blood vessels are destroyed by laser treatment. However, it is likely that 50 percent of patients with wet macular degeneration who receive this laser procedure will need a re-treatment within three to five years. You may be instructed to use the Amsler grid daily to monitor your vision for signs of change.
In some cases, a type of treatment for wet macular degeneration called photodynamic therapy, or PDT, may be an option. This therapy uses a combination of a light-activated drug called a photosensitizer and a special low-power, or cool, laser to treat wet macular degeneration right at the center of the macula.
This procedure is done on an outpatient basis, usually in an ophthalmologist’s office. The photosensitive drug is injected into a vein in your arm, where it travels through the body, including the abnormal vessels behind the central macula. The low-power laser light is targeted directly on the abnormal vessels, activating the drug, which causes damage specifically to those unwanted blood vessels.
After PDT, the abnormal blood vessels may reopen, so multiple treatments may be required.
It is important to remember that only about 10 percent of all macular degeneration cases are exudative, or wet form, and about 75 percent of these cases cannot be treated. People with wet or dry macular degeneration symptoms who cannot be treated will not become blind, as they will still have peripheral, or side, vision.
If you have untreatable macular degeneration, you can make the most of your remaining visionby learning to “see again” with the vision you do have and with the help of special low-vision rehabilitation, devices and services. People with low vision can learn new strategies to accomplish daily activities. These skills, including mastering new techniques and devices, help people with advanced AMD regain their confidence and live independently despite loss of central vision.
While there is little that can be done to improve the eyesight of someone who has AMD, with early detection, the rate of vision loss can be slowed. The keys to slowing vision loss are to understand macular degeneration, monitor your symptoms and visit your ophthalmologist regularly to test your vision. Even with macular degeneration, you can still maintain an enjoyable lifestyle.
With vision rehabilitation, people with low vision can learn new strategies to accomplish their daily activities. With new techniques and devices, people with advanced vision loss can regain their confidence and live independently.
People with low vision may find a team approach is often best in vision rehabilitation. This team may involve some or all of the following professionals:
This rehabilitation process can be a challenging and frustrating period of adjustment — one that requires patience, practice, motivation and the support of your doctor, low-vision specialist, family and friends. The rewards, however, can be great.
There are many devices specifically designed to help people with low vision function better. Different devices are available for different tasks. A trained professional can help you understand which device is best for accomplishing your particular needs. Training and practice are also important in order to become skilled at using any device.
Optical low-vision devices. Optical low-vision devices use lenses to magnify objects, making them easier to see. The lens strength will depend on your vision and the size of the object or print to be seen.
Magnifying spectacles. Stronger than ordinary glasses. They can be used for near tasks, such as reading, threading a needle, or any activity that requires detailed vision. The printed page or object must be held closer than usual in order to keep things in focus. One advantage of magnifying spectacles is that your hands remain free to hold reading materials or perform tasks.
Hand magnifiers. Familiar to most people and are available in varying strengths. Reading material is not necessarily held as close to the face as with magnifying spectacles, and some models come with a built-in light. High-quality and high-powered magnifiers are often available only in specialized stores or through vision rehabilitation professionals.
Stand magnifiers. Rest directly on the reading material, keeping the lens at the proper distance from the page. The ability to rest the magnifier on the page is useful for patients with a tremor or arthritis.
Telescopes. Used for seeing objects or reading signs that are far away. They can be handheld like a pair of regular binoculars or mounted on a pair of eyeglasses.
Video magnifiers. Electronic devices that use a camera and television screen to enlarge printed material, pictures, or small objects. They are adjustable and can enhance the material in different ways — for example, by making the print appear darker (increased contrast). The technology is developing rapidly, and electronic devices are becoming smaller, more portable and easier to use. Some can even be used for both distance and near tasks.
There are numerous low vision aids, devices, and techniques to help make everyday activities easier, including:
Good lighting and glare control are very important for people with low vision. A bright light should always be used when reading and its location should be adjusted for the greatest visibility without glare. Stronger light bulbs in darkly lit areas can make tasks like cooking, dressing, and walking up and down stairs easier. Wearing a hat with a wide brim or tinted wraparound sunglasses can shield your eyes from dazzling and annoying overhead lights or sunlight.
Macular degeneration reduces vision in the central part of the retina. It usually does not affect the eye’s side, or peripheral, vision.
People with AMD may have difficulty with daily tasks that require fine vision such as reading, dialing a telephone, driving, and recognizing faces.


